Terminal Sterilization Review | Terminal Sterilization Methods
Introduction to Terminal Sterilization:
The word terminal sterilization itself depicts its meaning i.e. terminal = at the end stage and sterilization means removal of living organisms from the product. This is by using one of the methods of sterilization processes. Normally sterilization is being done at various stages of the production process. Typically it starts with accessories sterilization, process optimization, component sterilization.
However, in a few aspects, final product sterility is the most important and prominent factor in the product lifecycle. It is ensured that throughout the product lifecycle the product content must be sterile.
Hence after manufacturing the product; finally, the complete product with its final container is subjected to sterilization and this process is called terminal sterilization.
1. Aseptic Processing:
Aseptic processing refers to the process in which the already sterilized items i.e. ready to use items are brought together and are aseptically assembled. This aseptic assembling is called aseptic processing. Normally aseptic processing is quite a common method for those products that are thermolabile.
2. Terminal Sterilization:
As mentioned in the introduction, it is the final stage of product processing and it is done to ensure the final product with its container is made sterile. Those products which are heat resistant for those this method works.
|
Terminal
Sterilization Aseptic Processing Difference |
|
|
Terminal
Sterilization |
Aseptic Processing |
|
Relies on a lethal treatment to microorganisms |
Relies on the removal/separation of microorganisms |
|
Safer |
More risky process |
|
Preferred by regulatory bodies |
Closely scrutinized by regulators |
|
Method of choice |
More widely used |
|
Degradation of materials always a concern |
Material quality/stability largely unaffected |
|
Easily reproducible process |
More variable process |
|
Relatively easy to validate |
Much harder to control |
|
Not for all materials |
No material issues |
|
Assumed more expensive |
Presumed less expensive |
Terminal Sterilization Methods:
A. Moist heat Terminal Sterilization:
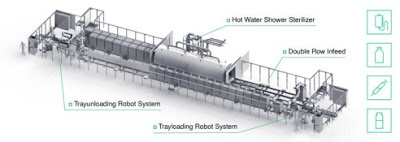
Terminal sterilization is a prominent factor for small volume parenterals, large volume parenteral, and ophthalmic products. Normally, in moist heat sterilization steam is used. However, in the terminal sterilization case, steam is not used as the terminal sterilization is done for the final product, so steam can degrade the product. Steam has more temperature. Hence in terminal sterilization instead of steam hot water is used.
However, it is ensured that desired F0 value is attained after hot water exposure. In steam sterilization, 121°C temperature for 15 minuted exposure is done. However, in terminal sterilization being less temperature more exposure time is required to achieve desired F0 value.
Reference:
2. Moist Heat Terminal Sterilization for Controlled Release Materials
B. Ethylene Oxide Terminal Sterilization:
Ethylene oxide terminal sterilization and radiation terminal sterilization are the most prominent factors of terminal sterilization and are being widely used in medical industries. However, for the ready-to-use products in the pharmaceutical industry, this method is used. For eg. rubber plugs, pre-sterilized garments, media plates, gloves. These accessories are opened in the pharmaceutical industry for further usage. But this method is not used for the final drug products in the pharmaceutical industry. As we decrease sterilization temperature, the exposure time will be increased.
In the ethylene oxide, chamber product is exposed to a validated combination of humidity, ethylene oxide gas, temperature, and time. For palletized products to drive humidity, deep vacuum cycles are often used. Before execution, it is ensured that the concentration of ethylene oxide gas, temperature, vacuum, and time is validated for the ethylene oxide chamber. EO levels are brought below permissible exposure limits through the completion of a validated in-chamber vacuum purge process or a post-sterilization aeration process. Product is released for distribution following review and documentation of routine monitoring parameters and, in many instances, biologic indicator test results. Total cycle times range from 6 hours to several days.
Ethylene oxide is a highly reactive cyclic ether with two carbons and one oxygen, CH2CH2O. It is a gas at room temperature with a boiling point of 11°C. It is pressurized and stored as a liquid for use in EO processing plants. The mechanism of microbial kill is the alkylation of the amine groups of DNA. Moisture facilitates microbial kill; as noted above, the product and thus the microbes must be exposed to a humid environment before EO exposure. The Ethylene Oxide kill rate is a function of the temperature and concentration of EO gas.
C. Radiation Sterilization:
Radiation sterilization accounts for most of the remaining 50% of the industrial terminal sterilization market. Fully functional finished good devices are placed and sealed within a sterile barrier packaging system according to defined product orientation. The product is loaded onto a conveyor system using a specified orientation and passed in front of a radiation source that emits electrons or photons that penetrate through the packaging and inactivate the device’s microbial load. One parameter, radiation dose, correlates directly with a microbial kill and is easily measured to provide process control. The mechanism for microbial kill is radiation-induced scission of DNA chains, either “direct” (i.e., direct scission of DNA chains) or “indirect” (i.e., scission mediated by formed radicals), which stops microbial reproduction. There are three radiation sterilization modalities: gamma, electron beam, and X-ray.
D. Gamma Sterilization:
Gamma sterilization uses cobalt-60, a radioactive element that undergoes nuclear decay-producing useful gamma radiation. These photons have a very large penetration capability, easily penetrating through two or more pallets of product. Racks of cobalt-60 rods provide the radiation source. A conveyor system moves many totes of fully packaged products into the sterilization chamber and around the racks, often passing by multiple times, to sterilize the product. The dose is related to the amount of exposure time the product experiences, typically ranging from 4 to 8 hours.
E. Electron Beam Sterilization:
Electron beam (E-beam) sterilization relies on high-energy electrons to accomplish sterility. Electrons are commonly accelerated up to 0.2 to 10 MeV and delivered as a continuous curtain or magnetically focused into a 1–5-cm-diameter beam that is magnetically scanned at high frequency across the product as it moves in front of the beam on the conveyor system. Low energy E-beam is used for surface sterilization of pharmaceutical packaging whereas high energy E-beams are used for fully packaged medical devices. Electrons from accelerators do not penetrate nearly as far as photons from gamma sources, so the product is often processed in single product cartons or small corrugated shipper boxes. Shown in Fig. is an illustration of a self-shielded E-beam accelerator and conveyor system. Products packed in corrugated shipper boxes are loaded on the conveyor system. Product is carried through the electron beam to achieve the desired irradiation dose, typically in a few seconds. The product is then returned sterile to an unload/product release station.
Reference:
Radiation and Ethylene Oxide Terminal Sterilization Experiences with Drug-Eluting Stent Products| Radiation sterilization | EN/ANSI/AAMI/ISO 11137-1 Sterilization of health care products—radiation—part 1: requirements for development, validation, and routine control of a sterilization process for medical devices |
| Ethylene oxide | EN/ANSI/AAMI/ISO 11135-1 Sterilization of health care products—ethylene oxide—part 1: requirements for the development, validation, and routine control of a sterilization process for medical devices |
| EN/ANSI/AAMI ISO 10993-7 Biological evaluation of medical devices, part 7: ethylene oxide sterilization residuals | |
| Moist heat (saturated steam) | EN/ANSI/AAMI/ISO 17665-1 Sterilization of health care products—moist heat—part 1: requirements for the development, validation, and routine control of a sterilization process for medical devices |
| Other | AAMI ST67 Sterilization of health care products—requirements for products labeled “STERILE” |
| AAMI TIR 17 Compatibility of materials subject to sterilization |
Terminal Sterilization Method Selection:
Terminal sterilization method selection is started by determining the desired sterility assurance level for the product packaged within the sterile barrier system. Product designed or assembled, in such a way that an interior surface of the product is nearly closed off to the external environment. If the product is exposed to terminal sterilization either the gas or any sterilizing medium will contact with the product, the product may degrade. To avoid this, closure of the final container before terminal sterilization is more important.
For terminal sterilization of ready-to-use products, closure of the final product is not recommended. This is to penetrate moisture and EO gas to reach and interact with microbes on the interior surface to destroy their DNA. If EO sterilization was desired, based on other factors influencing this choice, consideration could be given to how the product is assembled and packaged (e.g., if a stopcock is attached to a syringe, can the stopcock be left in an open position to allow moisture and EO gas to reach the inner surface of the syringe?). On the other hand, if a device includes active electronics, then radiation sterilization is not likely to be compatible.
An important and challenging step in selecting a terminal sterilization process would be to understand the compatibility of a product subject to a particular sterilization process. The chosen terminal sterilization method should achieve the desired F0 value to maintain the sterility assurance level. Product design, materials, and how the product/materials are manufactured are key compatibility factors to consider. However, it is recommended to consider that, after terminal sterilization, there should not be any changes to the physical and chemical properties of the product.
Conclusion on Terminal Sterilization Methods:
For pharmaceutical sterile dosage forms, terminal sterilization is the most widely used technique to get rid of bioburden. There are multiple ways of terminal sterilization, the suitable method to be selected based on final product properties. It is to be selected in such a way that, the physical and chemical properties of the final product shall not change.
Also, the selected terminal sterilization method shall achieve sterility assurance level by desired F0 value. This is to be validated before commercial use of the terminal sterilization method.


Any body can easily understand it. You describe it briefly with along 3D models. I am solving you problems and keep your food safe from pest through Residential Pest Control in New York. You can get to know more about it.
ReplyDeleteI am very impressed with your post because this post is very beneficial for me and provide a new knowledge to me.
ReplyDeleteTop 10 Pharma Franchise Companies in India
I am very impressed with your post since it is very useful for me and provides us with new information. technology review Blog
ReplyDeleteAbsolutely thanks for nourishing the necessary information. I appreciate to u, all are such good information, Thanks. Pharma Manufacturing Company in Lucknow
ReplyDeleteI saw you have unique knowledge of Pharma Products. Thanks for sharing such kind of information with us. VIT-Shield | VIT-Shield Medicines | VIT-Shield Ashwagandha 50mg tablets
ReplyDelete